Restoring lives
Every year, 23 million people worldwide are affected by heart failure. Many die while waiting for a transplant. An Australian man suffering from this condition spent 100 days with an artificial heart. This technological breakthrough from Australia could radically transform the lives of patients with heart problems.
By Barbara Smith, special correspondent, Hobart, Tasmania.
Suffering from severe heart failure, a 40-year-old Australian defied the odds by leaving St Vincent’s Hospital in Sydney with a titanium artificial heart. This pioneer lived for more than 100 days before receiving a transplant. This world first opens up new prospects for patients waiting for a donor. Designed in Australia, this heart implant, called BiVACOR, uses a rotary blood pump and magnetic levitation to replicate the natural blood flow of a heart. It allows patients with end-stage heart failure to survive while waiting for a transplant. Its operating life of more than 100 days in this case is still shorter than that of a donor heart, which can sometimes exceed ten years. Australian engineer Daniel Timms, who invented BiVACOR after his father died of heart disease, said he was happy to see decades of work bear fruit.
How does it work?
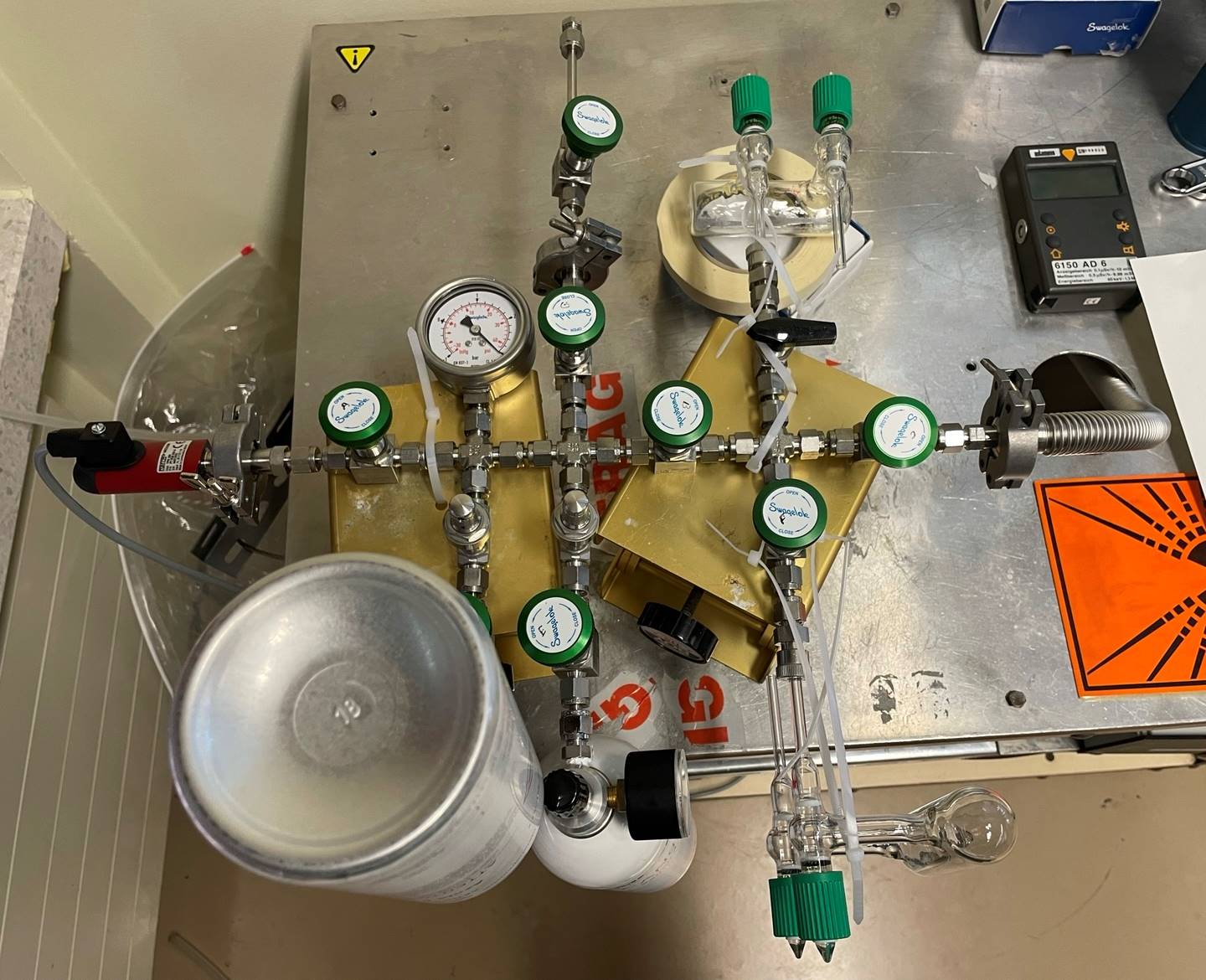
The BiVACOR total artificial heart has only one moving part, a levitating rotor held in place by magnets. It is made of titanium and has no valves or mechanical bearings that can wear out. It pumps blood to the body and lungs, replacing both ventricles of a failing heart. The long-term goal is to use this device to save more patients on endless waiting lists for a compatible donor. ‘Over the next decade, the artificial heart will become an alternative for patients who cannot wait for a transplant or when no heart is available,’ said Professor Chris Hayward of the Victor Chang Cardiac Research Institute, who oversaw the Australian patient’s recovery and helped prepare the device for clinical trials.
Three devices
The cardiac implant used on this Australian patient is part of a major medical programme: Artificial Heart Frontiers, led by Monash University. This programme aims to develop three major devices to treat the most common forms of heart failure. This procedure is the first in a series planned in Australia, marking a significant advance in artificial heart research. However, experts say there is still a long way to go before this technology can replace heart transplants.
Extensive trials
The first case dates back to July 2014, when a 58-year-old patient suffering from end-stage heart failure received the implant at the Texas Medical Centre. This allowed him to stay alive for eight days before a donor became available. Four other patients followed as part of this study, which examined the safety and performance of the device while they waited for a transplant. The trials will be extended to fifteen patients. The Australian implantation was the first in Monash University’s Artificial Heart Frontiers programme, worth nearly US$30 million.
The BiVacor cardiac implant uses a rotary blood pump and magnetic levitation to replicate the blood flow of a heart.